Root-Canal Therapy
Sometimes, due to extensive decay or physical injury, the pulp of a tooth (the living structure on the inside of a tooth that houses nerve fibres and blood vessels) may eventually get colonised by bacteria and get inflamed and infected. Most of the time this is a painful process, and since the tooth has a very limited capacity to heal, early intervention is recommended.
How does decay or injury affect the pulp?
Since the pulp is sheltered in the deepest layer of a tooth, it is only when a big cavity is allowed to progress unchecked that decay (colonies of bacteria and bacterial toxins) gets very close to the pulp. Bacteria and their toxins irritate the pulp, which gets inflamed. Following this, the pulp goes necrotic and a chronic infection sets in. Such an infection may be asymptomatic for a period of time, but may spontaneously flare up and cause a spreading infection of the tissues of the mouth and face, and feel tender to bite on.
What does a necrotic (infected) tooth feel or look like?
Even though some necrotic teeth do not give any symptoms and may be chance findings on a check-up or show up on a routine X-ray, most commonly affected teeth will start off giving non-specific symptoms of chronic inflammation, namely feeling sensitive to temperature change. As the inflammation gets irreversible, the tooth will feel intensely sensitive to hot and cold stimuli, and this persists for a few moments even after the stimuli are removed. At later stages pain might be sharp and stabbing in nature, and might even keep the patient awake at night. Following this, a latent period might set in as the nerve fibres die off and a chronic infection at the tip of the roots gets established.
Teeth which have had knocks on them rendering them necrotic may even turn dark as blood products on the inside decompose and discolour. If an abscess forms following a chronic infection, a necrotic tooth may feel tender to bite on, and on occasions, pockets of pus might be released via a sinus that looks like a raised spot on the gum beside the tooth. Sometimes an infection from a necrotic tooth may spread to the tissues of the mouth and the face which may be uncomfortable, or in worst cases life-threatening.
-
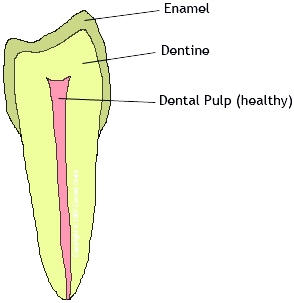
The Healthy Tooth
-
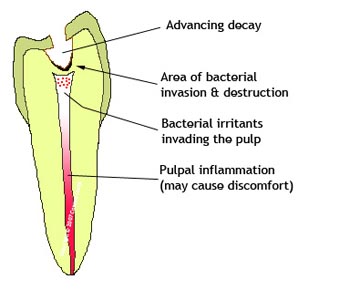
A Necrotic Tooth
The pulp may become necrotic and a chronic infection sets in. Such an infection may be asymptomatic for a period of time, but may spontaneously flare up and cause a spreading infection of the tissues of the mouth and face, and feel tender to bite on.
-
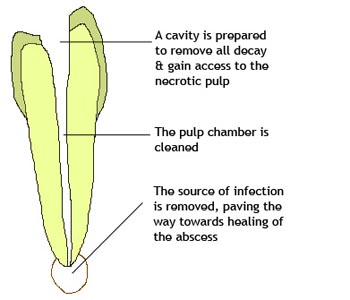
Root-Canal Therapy
Once infected, a necrotic tooth will not get better on its own, and the problem cannot be rectified with a simple filling. The aim of root canal treatment is to remove the dead pulp which is a source of chronic infection, as an alternative to having the whole tooth removed (extracted).
-
Root-Canal Therapy
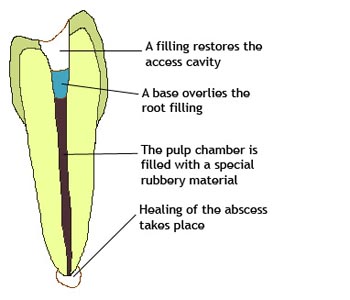
The root canal is disinfected using both mechanical instruments and chemical disinfectants until the infection is eradicated. Usually, the process is done over two or more visits, as the dentist may leave some disinfectant in the root canals for a while, to help the tissues heal. On the last visit, the root canals are filled again using a special filler, and a filling is placed on the tooth to restore normal function and appearance.
How does trauma lead to necrosis?
Physical injury, usually to front teeth, may result in necrosis or irreversible inflammation of the pulp for two reasons: the injury might result in a fracture of the affected tooth that goes through the pulp, thus exposing it to the bacteria that are naturally present in the mouth, following which the pulp gets infected. Otherwise the injury might displace the tooth, albeit transiently, resulting in severance of the blood vessels that supply the pulp. The pulp thus dies (goes necrotic) and in turn gets infected by bacteria that travel via the gingival crevice (margin between gum and tooth).
How does a RCT help save a necrotic tooth?
Once infected, a necrotic tooth will not get better on its own, and the problem cannot be rectified with a simple filling. The aim of root canal treatment is to remove the dead pulp which is a source of chronic infection, as an alternative to having the whole tooth removed (extracted).
The pulp chamber is first cleaned following the removal of all decay. The procedure is done under local anaesthetic, and after drilling into the tooth in the same way a filling is carried out, the dentist proceeds to disinfect the canals where the pulp was using both mechanical instruments and chemical disinfectants until the infection is eradicated. Usually, the process is done over two or more visits, as the dentist may leave some disinfectant in the root canals for a while, to help the tissues heal. On the last visit, the root canals are filled again using a special filler, and a filling is placed on the tooth to restore normal function and appearance.
We regret that due to safety concerns and the lack of appropriate portable equipment, we are unable to carry out root-canal therapy on a domiciliary basis, but we would be happy to refer any patients requiring such treatment appropriately.
Is there any after-care involved?
Sometimes, as the resulting cavity would be extensive following treatment, the dentist might suggest crowning a tooth to give it some extra structural support and prevent breakage.
Follow-up of root-treated teeth may involve taking radiographs of them periodically.
In certain complex cases, such as very slender curved roots, atypical canal shapes or failed previous root canal treatment, your dentist might suggest that the treatment be done at a specialist, which might guarantee a better success rate attributed to the use of specialist equipment such as microscopes.